Peripheral Vascular Disease (PVD)
PVD can be treated through a focus on controlling symptoms and slowing progression via lifestyle changes and medication, or through minimally invasive surgical intervention.
What is Peripheral Vascular Disease (PVD)?
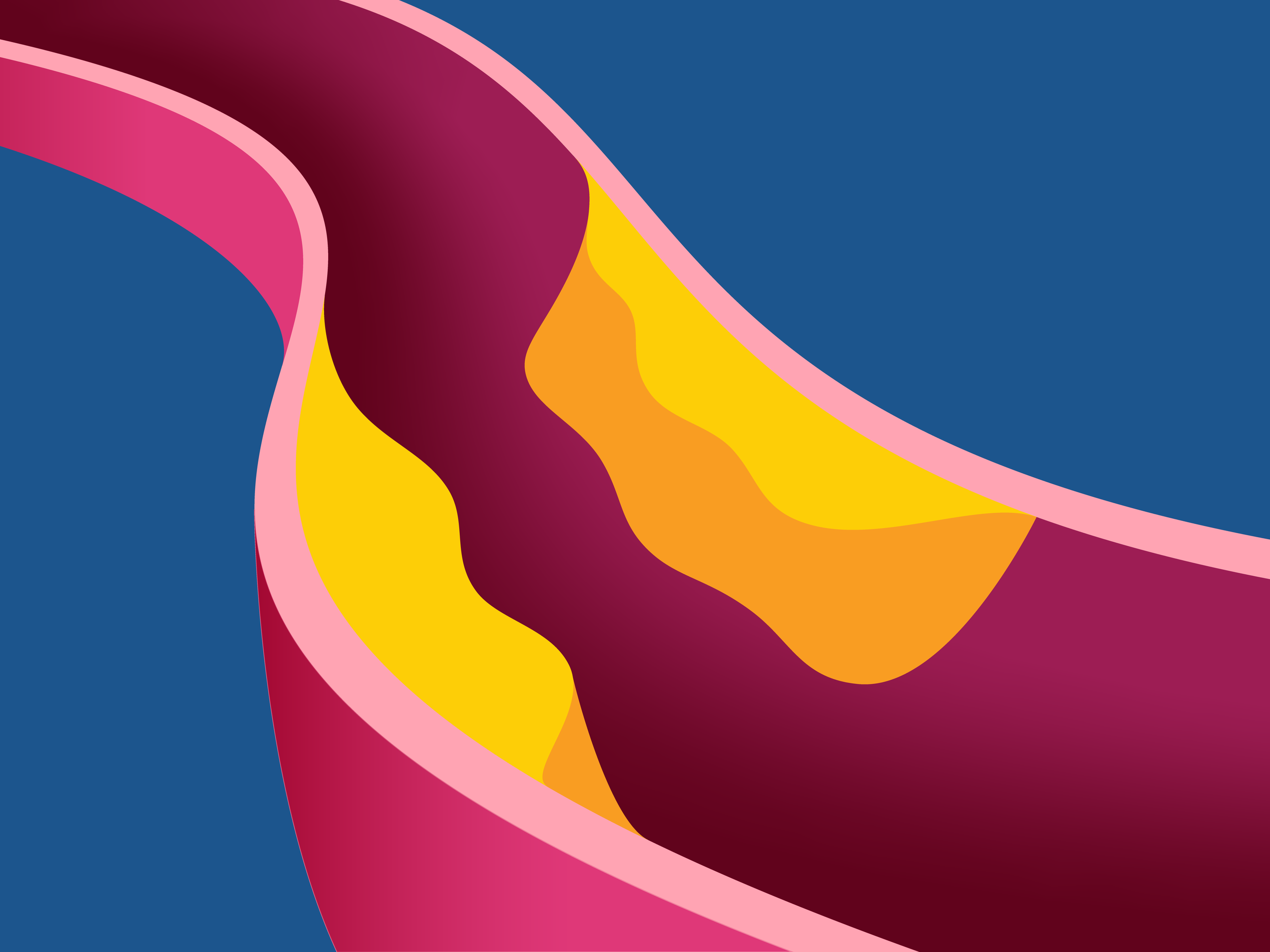
As someone ages, they are at higher risk of developing what is known as atherosclerosis, or hardening of the arteries. Basically, plaque builds up on the inner walls of your arteries, when low-density lipoproteins, the bad type of cholesterol referred to as LDL invades the artery wall.
Muscle cells in the wall of the artery overgrow and fat and calcium start to build up within these irregular spaces. Bleeding into the artery wall can also occur resulting in formation of a clot, which narrows the opening of the blood vessel even further.
There are many factors that can contribute to putting someone at risk of developing PVD:
Age greater than 50.
Male gender.
Diabetes or impaired glucose tolerance.
Postmenopausal women.
Family history of high cholesterol, high blood pressure, or PVD.
Coronary artery disease or heart disease.
High cholesterol.
High blood pressure.
Obesity or physical inactivity.
Smoking or use of tobacco products.
How is Peripheral Vascular Disease (PVD) diagnosed?
In order to confirm diagnosis, the physician uses a combination of physical examination and testing. Approximately half of patients with PVD are symptom free in the early stages of disease.
The most common first symptom reported is pain in the thigh, buttocks, or calf when walking. This occurs due to the lack of blood flow and oxygen to the tissue due to a narrowing or blockage in the blood vessels. In the early stages of disease, this pain will be relieved at rest, but once the disease progresses the pain will occur at rest as well.
Additional signs and symptoms for Peripheral Vascular Disease (PVD) may include:
Cool/cold feet to the touch.
Burning or aching pain in the legs while lying flat, that is relieved with sitting; often occurs in the toes at night.
Loss of pulse in the legs and/or feet.
Brittle, thin shiny skin and loss of hair on the lower legs and feet.
Non-healing wounds or ulcers over pressure points such as the heels or ankles.
Gangrene: darkened tissue that is dead due to lack of blood flow.
Loss of muscle or fatty tissue.
Impotence.
Numbness, weakness, or heaviness in muscles.
Restricted mobility.
Thickened, opaque toenails.
Reddish-blue discoloration of the extremities.
What are my treatment options for Peripheral Vascular Disease (PVD)?
Treatment depends upon the stage of the disease itself and focuses on controlling symptoms and slowing progression of the disease.
Lifestyle modifications would include quitting smoking, trying to maintain a healthier weight, and getting regular exercise such as walking at least 30 minutes, 3 times a week. Also, it is very important to control other risk factors by taking the appropriate prescribed medications to control blood pressure, cholesterol, and diabetes.
Medications prescribed by your vascular surgeon may include:
Trental or Pletal
These can help your blood flow easier through narrowed areas in your arteries, so they may help you walk longer distances without pain.
Aspirin or Plavix
These make your platelets less sticky, which lowers your risk of blood clots.
Statin Drugs
These will help keep your cholesterol levels better controlled, preventing further plaque buildup in your arteries.
In severe cases of PVD, lifestyle modifications and medications may not be enough to help with symptoms. In this instance, the vascular surgeon will determine the best surgical or minimally invasive treatment that is best for you. This will depend on your overall health, presence of other conditions, and the location and extent of blockages.
Angioplasty, Stenting, and Atherectomy
This is a minimally invasive procedure that involves inserting a long, thin flexible tube called a catheter through a small puncture over an artery in your arm or groin. Under x-ray guidance, this catheter is directed towards the blockage in the leg. A special balloon at the end of the catheter is deployed and deflated several times in order to compress the plaque against the walls of the artery. This widens the opening of the blood vessel, so blood is able to flow freely through it. In some instances, a mesh-like metal tube called a stent may be placed within the artery to keep it open. A device may also be used that cleans out the inner lining of the artery, removing the plaque by shaving or vaporizing it away, which is called atherectomy. These procedures can be performed outpatient, with only a short 4-hour recovery period before the patient can go home.
Bypass Surgery
Depending on the area of the blockage, incisions are made either into the leg, groin, or arm. The surgeon will use either a synthetic cylinder like tube called a graft or one of your own veins to reroute your blood flow around the blockage. The vein or graft is sewn above and below the area that is blocked, restoring blood flow to the tissues. This procedure requires a hospital stay of up to 5 days.
Endarterectomy
An incision is made into your leg or arm, depending upon the area of the blockage, and the plaque is removed from the inner lining of the artery. This opens the artery again, restoring blood flow to the leg. The effectiveness of this procedure depends upon the location and extent of the blockage. Hospital stay is about 3-5 days.
How can I prevent Peripheral Vascular Disease (PVD)?
PVD increases with age and from the progression of atherosclerosis from dyslipidemia, tobacco products, diabetes and hyperglycemia, obesity, and a sedentary lifestyle.
The progressive stenosis and occlusion, thrombus formation, or embolism of plaques or thrombi result in claudication, rest pain, and ulceration. Ulceration increases the risk of both local and systemic infection. Gangrene is the ultimate end-result, leading to amputation and life-threatening infection. Prevention is via mitigation of the risk factors other than age.
Dyslipidemia and lipid-lowering therapy: Alterations in diet and exercise and, when necessary, statin medication, to set goals of total cholesterol <200; LDL-C <130; and triglycerides <150.
Smoking cessation: Discontinuing cigarette use.
Diet: Management of hypertension with lifestyle changes (diet, exercise) and when necessary, anti-hypertensive medication.
Hyperglycemia: Strict glycemic control, especially in diabetic patients.
Antiplatelet therapy: Aspirin or clopidogrel (Plavix).
Exercise: Supervised exercise for claudication (exertional extremity pain).
Avoidance of medication: Avoid drugs that enhance hypercoagulation, such as estrogens in birth control pills or menopausal hormone replacement.
Counseling: A mental health professional can help identify causes of poor health choices and how best to change them.
Weight loss: Counseling with a dietitian/nutritionist is an important adjunct to the above measures and assures valid information upon which to base an individualized diet with reasonable expectations.
Revascularization: Once there is ischemic pain at rest, progression will continue until amputation unless there is intervention to improve perfusion, such as minimally invasive endovascular procedures (percutaneous) or open surgery.