May-Thurner Syndrome (MTS)
MTS can be treated via a combination of medication and minimally invasive surgery to reduce symptoms and reduce the risk of further complications.
What is May-Thurner Syndrome (MTS)?
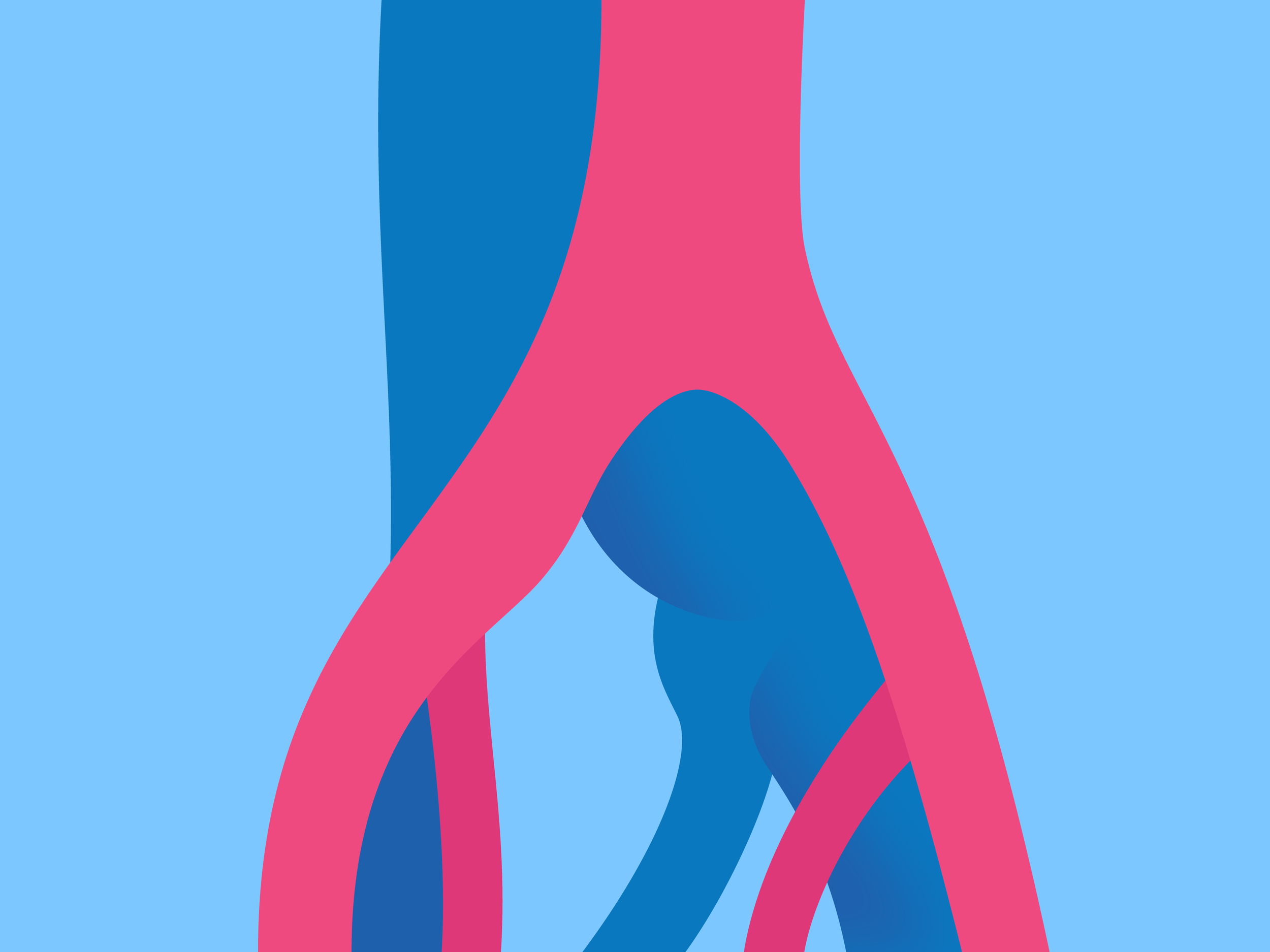
The iliac arteries originate from the largest artery in the body, the abdominal aorta. They split at the spine to form the left and right iliac arteries, which feed blood to the pelvis and legs. The right iliac artery is supposed to lie over the left iliac vein, but with this syndrome this artery is compressing the vein. As a result of this compression, the iliac vein narrows and constricts, sometimes scarring. This narrowing results in increased risk of developing blood clots or deep vein thrombosis (DVT) in that extremity.
Why do I have May-Thurner Syndrome (MTS)?
This condition is congenital but not hereditary and is more common in women than men. It shows up more frequently in young women taking birth control medication, as women age or as they gain weight. Many people may be unaware that they have this disorder, because many may only have some degree of compression of the iliac vein. Only a small number of individuals have severe compression of the iliac vein, resulting in symptoms, namely blood clots in the deep veins of the leg.
How is May-Thurner Syndrome (MTS) diagnosed?
Diagnosis is achieved by a combination of physical examination and diagnostic testing. Diagnosis may also occur when patients present with symptoms of a deep vein thrombosis (DVT) and further testing is completed.
Tests to confirm diagnosis include:
Duplex ultrasound.
Computed tomography (CT) scan.
Intravascular ultrasound.
Angiography.
What are my treatment options for May-Thurner Syndrome (MTS)?
The goal of treatment is to reduce symptoms as well as reduce the risk of further complications.
Anticoagulant Therapy
These medications thin your blood and prevent the current clot from increasing in size, as well as prevent new clots from forming. These medications do not dissolve the clots that you have. You may be on IV heparin for several days or an injection called Lovenox that is given in the abdomen once daily for 5 to 7 days. You will be started on a medication called warfarin (Coumadin), which is an anticoagulant pill. It can take about 3 days for this medication to have effect, so during that time you may be on both warfarin and heparin. You may be on this medication for up to 6 months, during which time routine blood tests are required to ensure your blood is at the appropriate thinness to prevent clots from forming.
Catheter-Directed Thrombolytic Therapy
During this procedure, a thin flexible tube called a catheter is inserted into a puncture in the skin and guided into the affected blood vessel of the lung. A thrombolytic drug is injected which dissolves the clot over a period of time. There is a much higher risk of bleeding as well as stroke with this therapy, compared to anticoagulants.
Angioplasty and Stenting
Once the clot has been removed from the vein, this procedure is performed to widen the compressed vein. A thin flexible tube called a catheter is inserted in a puncture over a vein in the leg. A small balloon at the tip of the catheter is inflated to stretch the iliac vein open, increasing blood flow to the leg. A small metal mesh tube called a stent is inserted through the catheter and guided to the ballooned area of the iliac vein. The stent will help hold the compressed area open and will remain in the vein permanently.
Inferior Vena Cava (IVC) Filter
During this procedure, a thin flexible tube called a catheter is inserted through a vein in your leg, arm, or neck. The vascular surgeon passes a small special metal filter through the catheter and places it in the inferior vena cava, which is a large vein in your abdomen that carries blood back to the lungs. This filter traps clots that break away from leg veins, preventing them from travelling to your lungs. This is done if the patient cannot tolerate anticoagulation therapy.
Can May-Thurner Syndrome (MTS) be prevented?
Since MTS increases risk of deep vein thrombosis (DVT) and complications associated with DVT, such as pulmonary embolism, prevention of these risks progressing to clinical events is prudent.
In the absence of DVT and for patients with only mild symptoms of left leg swelling or pain, conservative measures of prevention are used, specifically, compression stockings. These are also used if the severity of MTS requires more aggressive invasive interventions. Venous ultrasound imaging is helpful in ruling out more severe manifestations of MTS, such as DVT.
In advanced MTS that demonstrates signs and symptoms of advanced chronic venous insufficiency, such as limb swelling, pain, and skin discoloration, prevention of disease progression aims to reduce stenosis of the vein(s) using angioplasty and stents in the affected segments(s). Angioplasty alone results in a high recurrence rate. Thereafter, compression stockings are used.
In advanced MTS that results in venous thromboembolism (VTE), full anticoagulation therapy is begun (unless contraindicated by pre-existing coagulopathy). Catheter-directed or pharmaceutical thrombolysis is useful in eliminating the clots that may migrate. DVT requires anticoagulation according to the guidelines used in VTE prophylaxis.
Rarely, when more conservative or interventional measures are unsuccessful or contraindicated, an open cut-down may be necessary to evacuate the clot.
Prevention and follow-up utilize periodic venous ultrasound imaging.