Dialysis Access
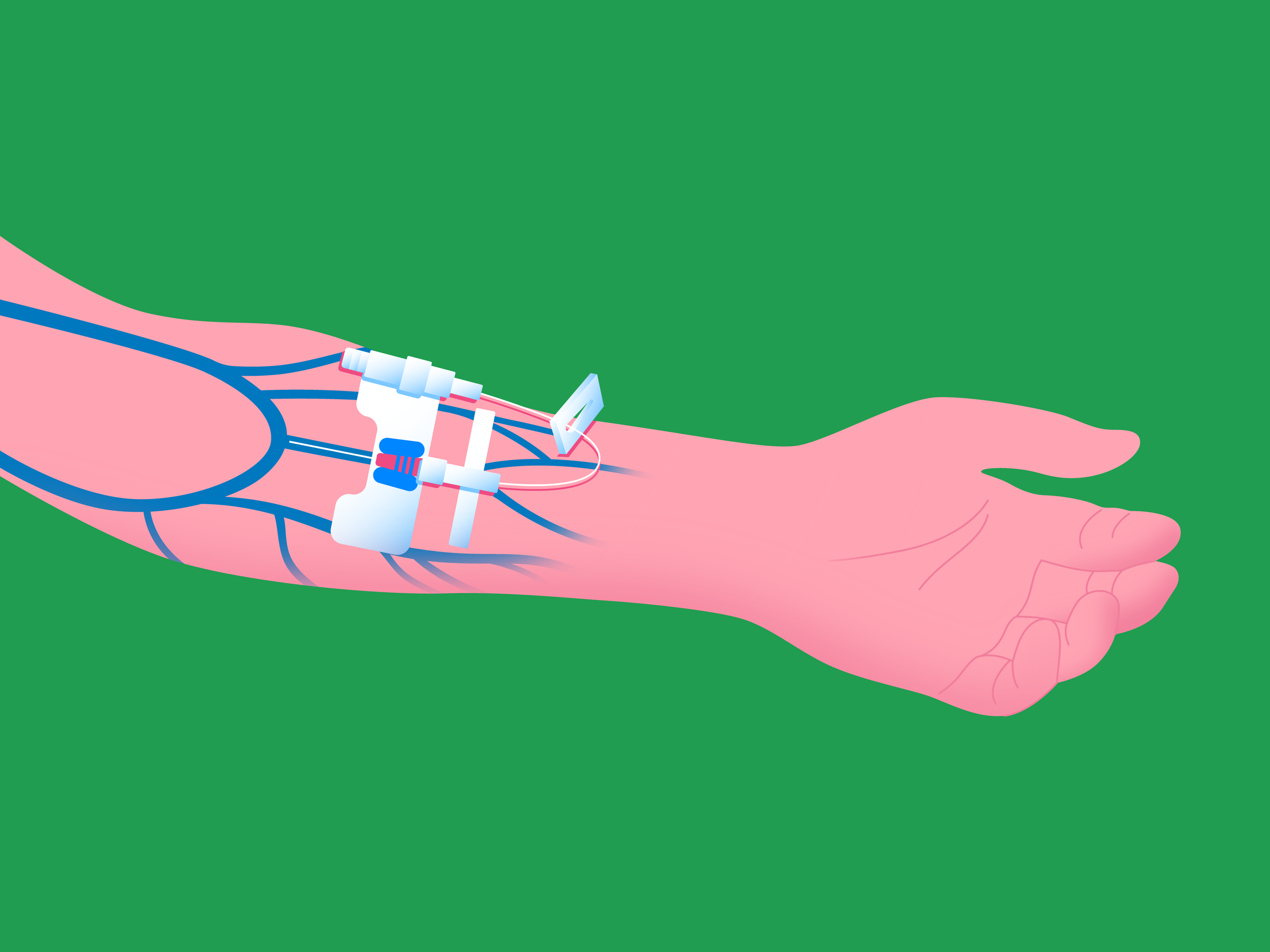
Dialysis requires temporary or long-term blood access sites via one of three types of minimally invasive surgeries.
What is Dialysis?
Dialysis is a blood-cleansing procedure performed routinely on patients who have acute or chronic kidney disease (CKD), or end-stage renal disease (ESRD). Kidney failure is most often irreversible, and options are dialysis or kidney transplant. In these patients, their kidneys have stopped functioning normally.
The purpose of the kidneys is to cleanse the body of waste products, regulate the fluid volume of the body and promote removal of the appropriate number of electrolytes and chemical substances. The process of dialysis is to do the job of the kidneys by cleansing the blood and removing waste products and excess fluid. In order to be hooked up to the dialysis machine, a blood access site must be created, that can withstand frequent needle puncture; these access sites can be temporary or long term.
What are the types of Dialysis Access Surgeries?
There are three types of dialysis access: central venous catheter, AV fistula (AFV), and AV graft (AVG).
Central Venous Catheter (Temporary)
During this procedure, a thin flexible tube called a catheter is placed into a large vein in the neck. This catheter can be used a maximum of 3 months, so long term dialysis patients will require something else eventually. Also, because this catheter is placed directly into the bloodstream, there is a high risk of infection.
A central catheter is not recommended for long-term use due to its risk of infection, which can be identified by evaluating leukocytosis with a complete blood count and differential and with periodic blood cultures.
In the arteriovenous access methods, thrombosis and stenosis can jeopardize the AV access point. In both AVF and AVG, testing for hypercoagulability can be done with blood tests that evaluate clotting capabilities. Repeat coagulations studies are warranted in high-risk graft patients undergoing anticoagulation therapy.
AVF
During this procedure, a small incision is made, and an artery and a vein are sewn together. About 6 weeks following the procedure, the vein will increase in size and become thicker and tougher.
After creating an endogenous AVF, its maturity for use can be accessed via imaging studies such as ultrasound. Stenotic lesions, thrombosis, or aneurysm formation that threaten the lifespan of a usable AVF are also evaluated via ultrasound.
AVG
During this procedure, two small incisions are made in the arm and a cylinder like tube called a graft is inserted under the skin. One end of the graft is sewn to the artery and the other end to the vein. Again, this increases the size of the vein and it becomes tougher and thicker, with rapid blood flow from the artery to the vein.
Stenosis, thrombosis, and pseudoaneurysm (defects due to repeated cannulation) are also evaluated via ultrasound.
It is the indwelling central venous line that poses the greatest risk of infection. Nevertheless, the AV methods are not immune and may require blood work to rule out signs of infection, such as elevation in WBC or positive blood cultures.
Regardless of which type of access is used, the lifespan of the access is jeopardized by
Stenosis.
Thrombosis.
Infection.
Ruling out these complications via monitoring is necessary on a continuing basis.
The usefulness of dialysis access is dependent on its patency, and any of the above three complications can interfere with or completely eliminate the patency that the access requires. Patients can check for a “thrill,” which is a palpable sound–the tactile perception of circulatory turbulence–within the dialysis access. Absence of a thrill indicates blockage from stenosis or thrombosis.
How do I know if the AV Graft (AVG) is functioning effectively?
There are two signs that indicate a dialysis access site is functioning well. When you slide your fingertips over the site you should feel a gentle vibration, which is called a “thrill.” Another sign is when listening with a stethoscope a loud swishing noise will be heard called a “bruit.” If both of these signs are present and normal, the graft is still in good condition. If not, there may be a narrowing within the graft as a result of blood clot collection. If there is bruising or discoloration close to the graft site, this could indicate that part of the graft wall was punctured and may require repair as well. The site may need to be reopened and repaired, or it may be possible to insert a thin flexible tube called a catheter through the site and use a balloon to widen the opening of the graft and improve blood flow.
What are signs or symptoms I should report?
It is very important to protect your dialysis access site! Do not compress the arm containing the site with tight clothing or jewelry and do not rest anything heavy against it. Remember that it should never be used for routine blood draws, as an IV site for medications or fluids, or as an arm for blood pressure cuff readings. Signs or symptoms that are potentially dangerous and need to be reported include:
Signs of infection at the access site, such as redness, swelling, or drainage of pus.
A large bruise spreading away from the graft site following a recent dialysis session.
A pulsating hard knot under the skin.
Lack of bruit or thrill.
Coldness, paleness, aching, or tingling in the extremity with the access site.
How do I prevent Dialysis Access Failure?
The complications that can cause dialysis access to fail include:
Stenosis.
Thrombosis.
Infection.
Distortion due to the damage from repeated cannulations (pseudoaneurysm). While ultrasound can identify the stenosis, thrombosis, and anatomical distortions, it cannot prevent them.
Infection is best prevented by conversion from a central venous line to an arteriovenous approach. Infection in arteriovenous fistulae or grafts are best prevented with the mandatory aseptic technique during the cannulation process, using sterile precautions and antiseptic cleansing, and gloves and masks. Patients and clinicians alike can examine the fistula or graft site for redness or undue tenderness.
Most stenosis occurs due to an injury at the site of stenosis. Thrombosis can also jeopardize the patency that any dialysis access requires. Two simple tests can provide reassurance that all is well:
Palpation of a thrill: Which is the tactile feedback of turbulence in the fistula or graft.
Listening for a bruit: Which a clinician hears with a stethoscope.
A thrill or a bruit is an indication that the site is communicating well between arterial and venous circulations.
Patients at high risk for thrombus formation can use anticoagulant therapy to prevent this.