Diabetic Retinopathy (DR)
DR is the main cause of impaired vision for those between the ages of 25-74. The macula, an oval-shaped pigmented area in the central retina responsible for high-resolution and the color vision, can develop edema; the entire retina is at risk of rogue blood vessels hemorrhaging into the retina or causing it to detach.
What is Diabetic Retinopathy (DR)?
DR is the main cause of impaired vision for those between the ages of 25-74. The macula, an oval-shaped pigmented area in the central retina responsible for high-resolution and the color vision, can develop edema; the entire retina is at risk of rogue blood vessels hemorrhaging into the retina or causing it to detach.
Diabetes Mellitus (DM) and Diabetic Retinopathy (DR)
Most patients with DR have no symptoms until its latest stages, making screening a priority in preventing it. In type 1 DM, DR begins within 5 years of their diabetes diagnosis; in type 2 DM, DR onset can take as long as 20 years.
The hyperglycemia of diabetes is toxic to vascular tissues along two scales:
Macrovascular (atherosclerosis leading to cardiovascular disease).
Microvascular (DR, nephropathy, and neuropathy, i.e, vision, kidney, and cognition).
Type 1 diabetes mellitus (DM) causes damage more quickly and earlier than in type 2 DM, in which complications can be more insidious and diagnosis delayed.
Vision in diabetics is at risk due to refractive (correctable) errors, cataracts, and glaucoma, all of which are more common in diabetics. DR (disease progression in the retina) can result in blindness.
Neovascularization
There are two main forms, based on whether or not there are abnormal new vessels:
Nonproliferative DR (NPDR)
Nerve-fiber infarcts at various layers give a “cotton wool” spottiness to the retina. Retinal hemorrhages, microaneurysms, occluded vessels, and dilated/tortuous vessels appear in the macula and posterior retina. Visual loss, however, is primarily due to macula edema.
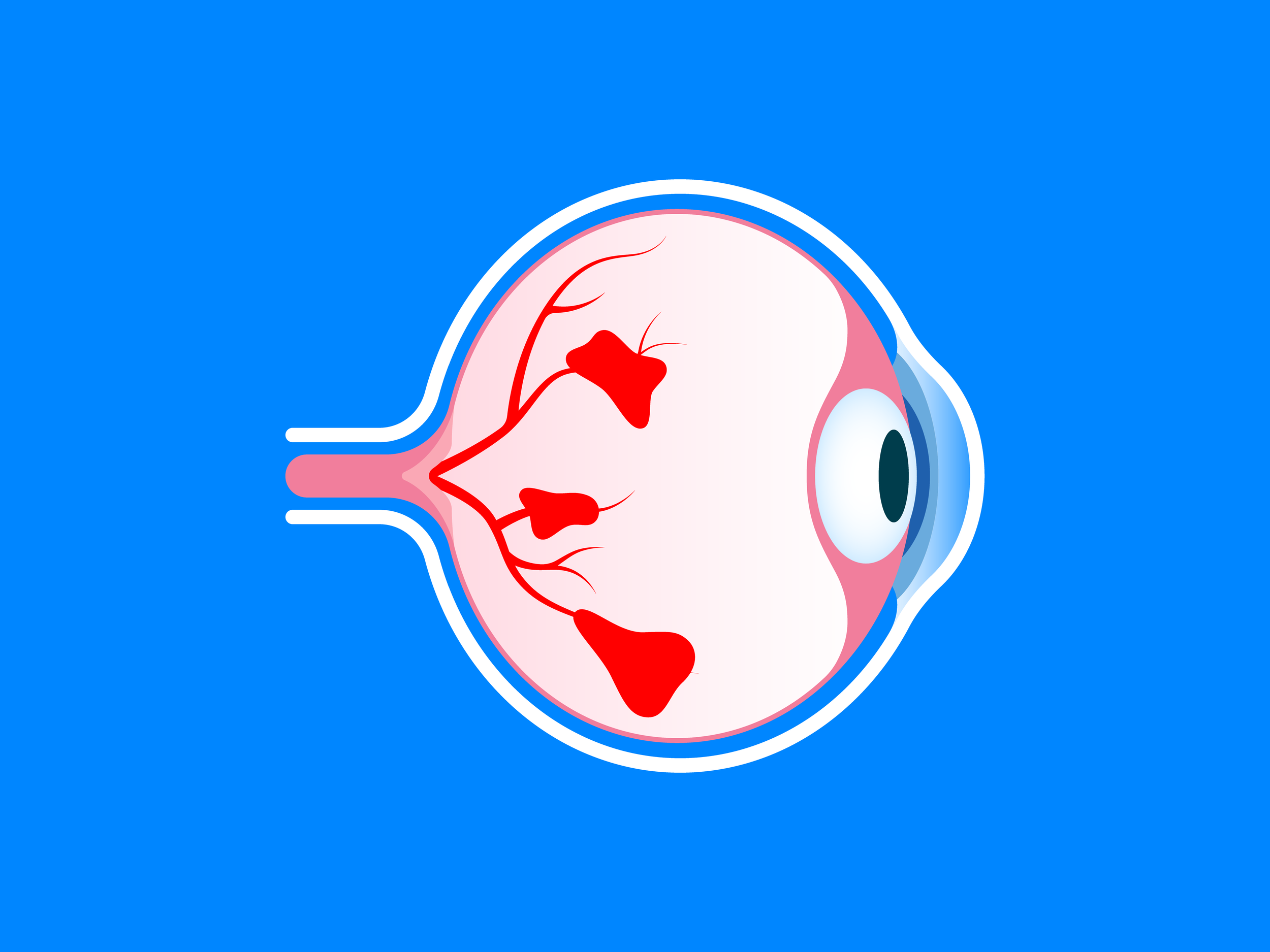
Proliferative DR (PDR)
There is neovascularization, along with its complications–vitreous hemorrhage, fibrosis/scarring, and tractional retinal detachment. Neovascularization involves fragile new vessels which rupture, causing hemorrhage within the eye. Visual loss, due to blood blocking the path of light through the eye to the retina, can be temporary until the blood clears, while retinal detachment causes permanent vision loss. PDR can also create a fibrovascular overgrowth that can distort the retina to the point of detachment.
How is Diabetic Retinopathy (DR) diagnosed?
Since DR typically won’t have symptoms until so late in its progression that any successful treatment is unlikely, the best diagnostic approach is via screening. Early detection of changes that are unnoticed by the patient can allow early treatment to be more beneficial.
Screening can be done by an ophthalmologist or an appropriately trained specialist, and thereafter serial retinal photographs can be used to follow the progress of eye conditions. Ophthalmoscopy with the help of pupil dilation is used in conjunction with retinal photography.
Type 1 diabetes mellitus (DM) is diagnosed more quickly than type 2 DM which has an insidious onset. This allows type 1 DM to be diagnosed earlier, before any eye damage occurs. Initial screening in type 1 DM should begin within 3-5 years of diagnosis; it is unusual for retinopathy to begin before that.
With type 2 DM, due to its insidious onset, eye damage may already have occurred by the time of diagnosis, so screening should begin immediately upon diagnosis. If there is no retinopathy, repeat screens can be done every 2-3 years; if there is, then annual exams should be scheduled.
Pregnancy with pre-existing diabetes accelerates the progression of any retinopathy, so women with diabetes should have comprehensive eye exams before any planned pregnancy or immediately if pregnancy occurs first. After delivery, screens should be done more frequently than in diabetics without a recent pregnancy.
The frequency of screening should be individualized, based on the presence or absence of abnormal findings or retinopathy.
Management of Diabetic Retinopathy (DR)
Chronic hyperglycemia is the cause of the DR that occurs in diabetes. The diseased tissue of the retina provokes the growth of new vessels from adjacent ones in an attempt to revascularlize it. Therein is the problem: neovascularization engenders the risk of hemorrhage and tractional retinal detachment.
The importance of early diagnosis of DR makes more likely any benefits from its management and treatment. Treatment is based on whether the retinopathy is nonproliferative (NPDR) or proliferative (PDR).
Nonproliferative Diabetic Retinopathy (NPDR) Treatment
Macular changes are the main cause of visual loss in NPDR. Macular edema or ischemia, when severe, are treated by using intravitreal antivascular endothelial growth factor (VEGF) in the eye under anesthesia. Alternately or in combination, laser photocoagulation can seal suspicious blood vessels before they hemorrhage or create traction on the retina. The goal of treatment is preservation of remaining vision while reducing progression. Macular edema also responds to injected steroids as a treatment alternative.
Proliferative Diabetic Retinopathy (PDR) Treatment
This more progressive condition mandates more aggressive treatment. Panretinal photocoagulation is the primary treatment for severe PDR and has been shown to reduce visual loss significantly.
If retinal detachment occurs, removal of the vitreous (“vitrectomy”) helps reach the goals of therapy by stabilizing the intraocular environment. Anti-VEGF inhibitors are useful, also.
Complications of panretinal treatment:
Pain.
The increased intraocular pressure of a temporary glaucoma.
Corneal abrasions.
Macular edema, loss of visual acuity, loss of dark adaptation.
Hemorrhage.
In this aggressive treatment, the benefit outweighs the risks.
How can I prevent Diabetic Retinopathy (DR)?
The prevalence of DR increases with the duration of the diabetes. Instability of glycemic control of diabetes is an important factor in DR’s appearance, progression, and severity, and the stability of strict glycemic control is the optimal way to favorably impact prevention.
Comorbid contributions to the progression of both the diabetes and complications such as DR result from hypertension, smoking, lipid abnormalities, kidney disease, and pregnancy. Treating these effectively improves the composite status to which they all contribute.
Prevention overlaps with treatment:
Strict glycemic control in the early course of diabetes is necessary to prevent or mitigate DR.
With retinal pathology, photocoagulation (laser) for vision-threatening DR is indicated.
Vitrectomy.
Intravitreal drugs.
Prevention
Prevention relies upon the recognition of the risk factors for DR. Frequent lapses in strict glycemic control that cause hyperglycemia, as well as hypertension, raise the risks for developing it. Effective prevention relies upon the following:
Good diabetic management via strict glycemic control, according to the goals established by the doctor.
Antihypertensive therapy for those with hypertension.
Lipid-lowering therapy, using statins.
The benefit of lipid-lowering of improving overall cardiovascular status indirectly benefits patients with DR in that it increases their survival when there are conditions that contribute cardiac risk.